As March is national social worker month, VetAssist Regional Manager Dana Taylor, LCSW, is sharing three case studies involving safe discharge planning for senior patients leaving a hospital or rehab facility for home. Veterans Home Care salutes social workers especially those who work in geriatric care, senior housing, medical social work, or clinical social work. The case studies describe how social workers successfully helped older adults find resources to return home safely.
“I work with some of the most dedicated social workers you will ever meet,” says Dana Taylor. “Social workers are a close-knit group. We network with each other to find the support our patients and clients need.”

Dana, whose practicum for her masters degree included hospital social work, joined Veterans Home Care in 2008. She says patients can be very vulnerable leaving an inpatient care setting to return home, especially if they live alone as do many older adults.
Social workers are key to bridging the gap through discharge planning. Family members are often stressed to learn that hospital stays require a medical necessity. When patients are medically stable, but not fully able to care for themselves, a hospital may discharge the patient. Medical need is assessed by taking a patient’s vital signs such as: body temperature, heart rate or pulse, respiratory rate, blood pressure, oxygen saturation level, and blood glucose level. Doctors may also consider pain level, state of mind and other factors to ensure a patient is safe to leave. However, families can’t rely on hospitals to provide custodial care for medically stable patients.
Custodial care is different from medical or skilled care. Often, social workers must explain the difference to patients and their families. Custodial care is needed when a person needs help with activities of daily living or ADLs. Discharge planning includes identifying if custodial care such has help with bathing, dressing, food preparation and mobility are needed.
Sometimes family members or neighbors can help someone transition from hospital to home. Another option is a private-duty home care aid which is often covered by long term care insurance but not typically covered by health insurance or Medicare. Sadly, most older adults do not have additional long term care insurance.
“Often, people assume Meidcare pays for in-home care and are shocked to learn that it doesn’t,” says Dana.
Discharge planning may include physical therapy or physical rehabilitation. Doctors often prescribe “PT” or “rehab” so discharge planning will include a referral to a therapist or finding a bed at a skilled nursing facility that offers rehab services.
When a patient leaves the hospital to care in a skilled rehab center, they also receive the custodial care they need including meals, help using the bathroom, bathing assistance and more.
Case Studies Where Social Workers Made A Lasting Impact Through Discharge Planning
The following three case studies show successful outcomes and a continuum of care that helped patients avoid an unnecessary hospital re-admission. In all three cases, the social workers found a permanent solution for their patients to return to their homes with private-duty in-home caregivers.
The patients were referred to Veterans Home Care’s VetAssist Program. VetAssist provided free consultation and help with the VA application for veterans’ benefits. The patients were charged the market rate for care by a home care agency in the VetAssist provider network.
In each case, the social workers remembered to ask about the military status of their patient. It is especially important to ask female patients who may not have served but may be a veteran’s wife or widow. The questions to ask are:
1. Are you a veteran or the surviving spouse of a veteran?
2. Did you (or the veteran) serve during wartime? Overseas service, combat duty or a service-related disability is not required.
3. Did you (or the veteran) receive an honorable or general discharge?
When the patients said, “yes” to these questions, the social workers
referred their patients to the VetAssist Program.
CASE 1- Korean War Veteran Albert Warren
Case 1 Situation: Albert was happily married for 65 years until his wife Shirley passed away May 23, 2019. In 2013, he was a patient at Avante Rehab in Irving, Texas. After rehab, he would require help at home.
Case 1 Solution: His social worker approached him at his dinner table one evening and asked if he had been in the military. He proudly mentioned his Air Force service in 1952-1956 during the Korean War. The social worker then referred him to the VetAssist Program to help him receive VA benefits for care at home.
Case I Outcome: Mr. Warren received in-home care through the VetAssist Program for seven years. He passed away on Thanksgiving night, November 26, 2020 at age 86.
Albert Warren’s daughter Patricia Snider says her family is grateful for the social worker who treated her father with respect, knew about the VA Aid and Attendance benefit and referred him to the VetAssist Program. “I will continue to recommend Veterans Home Care. This organization has been a blessing for our family.”
CASE 2- Veteran’s Surviving Spouse Catherine DeNova

Case 2 Situation: At age 90, Catherine DeNova lived and relied on her daughter, Lynn Opuda, for around the clock care. Catherine had a pacemaker and suffered from congestive heart failure. Catherine was the surviving spouse of a WWII veteran. Even though her husband died in 1977, she was eligible for a little-known benefit from the Department of Veterans Affairs. Her daughter already knew about the VA Aid and Attendance benefit and attempted the application process but was too busy with her mother’s daily care to finish it.
Case 2 Solution: During a stay at Chilton Hospital in New Jersey, the family met Beth Aymar, LCSW, who assessed the situation and knew both Mrs. DeNova and her daughter Lynn needed help. Beth referred them to the VetAssist Program.
Case 2 Outcome: Mrs. DeNova returned home to live with her daughter and received about 9 ½ hours of care per week. Her daughter said she was thankful that the social worker hooked her up with the VetAssist Program to complete all the paperwork and arrange for caregivers.
“It was a blessing for us both. It not only changed my mother’s life. It changed mine. I’m so grateful for our social worker and for VetAssist,” said Lynn. My mother had two different caregivers, Yun and Ulyana, from a VetAssist network provider and loved them both.”
Catherine happily taught her first caregiver, Yun, how to crochet. She had a close relationship with both caregivers who painted Catherine’s nails and did jigsaw puzzles with her. In home care improved Catherine’s quality of life and gave her daughter respite care. Mrs. Denova continued receiving her VA benefits for private duty home care for almost two years before she passed away.
CASE 3- WWII Veteran Robert Benden
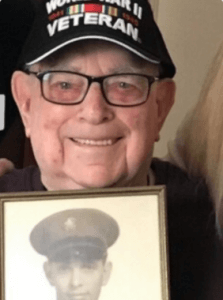
Case 3 Situation: At age 99, Robert Benden, a cancer survivor with a pacemaker, did remarkably well using a walker. He even lived alone in New Jersey with help from his daughters nearby. They did his laundry and shopping and checked on him. During a hospital stay, his social worker realized this family could benefit from a home care aide so she put him in touch with Mitch Miller, LCSW, at Valley Home Care part of the Valley Health System.
Cases 3 Solution: Mitch knew that Mr. Benden, as a WWII veteran, was eligible for the VA Aid and Attendance benefit even though Mr. Benden hadn’t suffered from an injury during his military service. He referred the family to the Vetassist Program. With VetAssist, care starts right away. The family doesn’t have to wait for the VA do adjudicate the claim and funds to arrive. At age 99, there was no time to waste.
Case 3 Outcome: Mr. Benden’s daughters called right away and with help from the VetAssist team began gathering the paperwork. Mr. Benden’s home care began in and his application for benefits was sent to the VA in Februay 2019. VetAssist provides a free loan so that the client can pay for care right away. When the VA processed the claim and funds arrived in May 2019, the amount was retroactive to February 2019. So he was able to repay Veterans Home Care for the care he already received.
Robert’s daughter, Kitty said her father loved his home care aide. When his caregiver was house-hunting, Mr. Benden enjoyed driving along as a passenger to look for houses. Robert Benden had almost two full years of VetAssist service before his died at 101.
If you are a social worker and would like to learn more about the VetAssist Program, call 877-390-6377 or email info@veteranshomecare.com. To refer a client, friend or loved one to the VetAssist Program, call 888-314-6075 or complete our referral form. To check someone’s eligibility for the VA Aid and Attendance and the VetAssist Program, click here.














